In Regione Caecorum Rex Est Luscus - Towards routine clinical examinations of joint kinematics.
Scott A. Banks, PhD and Paris. D.L. Flood, MSc
Department of Mechanical & Aerospace Engineering, University of Florida, Gainesville FL, USA
Email: banks@ufl.edu
Have you considered the terrible irony that the singular purpose of our joints is motion, yet we routinely assess joint injuries and diseases with static, non-weightbearing methods? This is not due to lack of interest from our clinical colleagues, but from lack of technology providing accurate, practical and low-cost technology to quantify dynamic joint-motion in a routine clinical setting. If we could provide such technologies in a cost-effective manner, there is almost guaranteed beneficial utilization in an array of orthopaedic scenarios.
Radiographic image-based spatial measurements have been performed essentially since the time of Roentgen, with our colleagues and forebears in the RSA community having brought these methods to practical use in orthopaedics and biomechanics. We now utilize an array of Roentgenographic imaging and measurement methods to quantify displacements of bones and implants over multiple length- and time-scales for the purposes of research. These techniques have proven invaluable in advancing implant designs and fixation methods, surgical methods and as support for computational simulations. However, there currently are no radiographic methods in routine clinical use for the purpose of quantifying joint kinematics/mechanics in a diagnostic or follow-up characterization role.
Single-plane fluoroscopic or digital flat-panel imaging have been used for the past 30 years to quantify joint and implant kinematics in a wide range of studies. There now are a variety of image-analysis methods, including open-source and commercial codes. However, to our knowledge, none of the reported methods are completely autonomous, with all requiring a human user to provide some initial guess(es) on bone or implant pose to start numerical optimization for model-image registration. This requirement for human supervision is a primary impediment to moving these measurement techniques into clinical use – they represent a substantial cost and workflow requirement that would be cost-prohibitive in the current health-care environment. If these measurements can be made fully autonomously, then having a surgeon order a ‘motion study’ for a patient with an unstable shoulder or a problematic ACL reconstruction may become feasible.
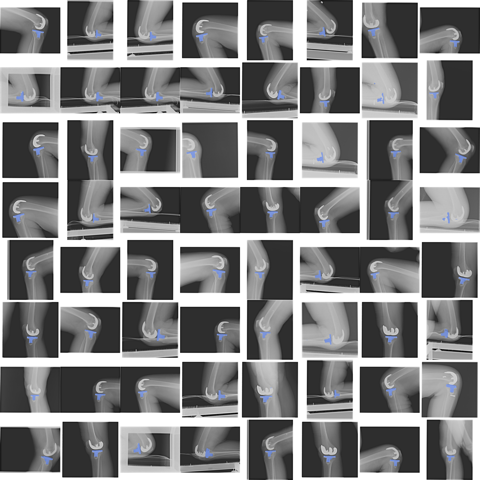
This presentation will focus on two ongoing efforts. First, a new open-source model-image registration platform with very robust numerical performance has been introduced. Current efforts are exercising this tool to validate its performance compared to previous methods and results, and to explore study-specific cost functions to enhance measures over a range of exams. Second, machine learning using convolutional neural networks is being explored to eliminate the need for human-supervised pose initialization and make the entire model-image registration process autonomous (Fig. 1). Results of both lines of effort will be presented to provoke discussion and seed potential collaborative efforts among the participants towards future clinical applications.
Disclosures: None.
Acknowledgment: The developments reported herein have been supported by a grant from The McJunkin Family Charitable Foundation.
Scott A. Banks, PhD received bachelor and master of science degrees in biomedical engineering from Case Western Reserve University, Cleveland, Ohio, in 1985 and 1988. Dr. Banks received the doctor of philosophy degree in mechanical engineering from the Massachusetts Institute of Technology in 1992. For his doctoral work, Dr. Banks developed a technique to measure three-dimensional motions of knee replacements from their two-dimensional projections in x-ray video sequences. Applications of this technique, and further developments thereon, have been the focus of Dr. Banks' work since 1992, contributing to a new generation of increasingly durable and high function knee implants. At the University of Florida, Dr. Banks teaches graduate and undergraduate courses in biomechanics, controls and robotics, and directs graduate students on a range of human and animal biomechanics studies and new technology related projects. Dr. Banks has coauthored over four-hundred peer-reviewed journal articles, conference papers, and book chapters and he is active on the editorial board and review staff of numerous orthopaedics and biomechanics journals. In 2013 Dr. Banks served as the President of the International Society for Technology in Arthroplasty and was elected into membership in The Knee Society. Dr. Banks has lectured or performed studies in more than 20 countries and works with orthopedic manufacturers worldwide to bring advanced treatments to patients. Dr. Banks enjoys research collaborations throughout the world and relishes the challenge of improving clinical outcomes in diverse cultures through the application of technology and engineering principles.
Outside of work, Scott is active training for his next backpacking expedition and obsessing over which lightweight gear to carry. In 2018, Scott completed the Tour du Mont Blanc with his wife Anne, and solo-hiked the John Muir Trail.
 Professor Dr. Ir. Nico Verdonschot
Professor Dr. Ir. Nico VerdonschotNico Verdonschot1,2, Dennis Janssen1, Marco Marra2 and Sebastiaan van de Groes1
1) Radboud University Medical Center, Orthopaedic Research Laboratory
P.O. Box 9101, 6500 HB Nijmegen, The Netherlands
e-mail: nico.verdonschot@radboudumc.nl
2) University of Twente, Laboratory for Biomechanical Engineering, Enschede, The Netherlands
Abstract:
It is highly important to stimulate innovation in artificial joint replacement technology. Particularly for the younger patient there is no life-time solution to treat their degenerated joints. Furthermore, clinical outcomes are satisfying for every patient. Clinicians, researchers and companies work together on generating new implant designs, surgical techniques and post-operative evaluation methods. To reliably test new innovations requires long-term clinical studies. RSA studies have been shown to be effective to detect implants with design-flaws in rather small groups of patients. To further minimize risks of exposing patients to inferior implants and technologies predictive modeling can be applied in many cases. Using musculoskeletal and finite element computer models our laboratories in Nijmegen and Twente are collectively working towards developing workflows that test implants and technologies at a pre-clinical stage. In this presentation we will illustrate how we test and co-design implants with companies and clinicians. Examples will be the development of an artificial meniscus prosthesis, a PEEK femoral TKA component and personalized surgical functional pre-planning of patella-femoral problems.
Present position
· Scientific Director of the Technical Medical Centre, University of Twente
· Head of the Orthopaedic Research Laboratory, Radboud university medical center, Nijmegen, the Netherlands
· Full professor, University of Twente, Enschede, the Netherlands
· Full professor, Orthopaedic Research Laboratory, Radboud University Nijmegen Medical Centre
· Visiting professor at the Politecnico di Milano, Italy
· Honorary doctor at the Aalborg University, Denmark
International esteem
· Over 300 publications in the peer reviewed literature
· Over a 100 invited lectures at international meetings
· Supervisor of 18 ongoing PhD students
· Chairman of the Orthopaedic Implant Section of the Orthopaedic Research Society
· Chairman of the Award committee of the International Society for Technology in Arthroplasty
· Board member of the International Combined Orthopaedic Research Society
· Honorary member of the International Society for Technology in Arthroplasty
· Elected fellow of the International Combined Orthopaedic Research Society
· Past president and honorary lifetime member of the European Orthopaedic Research Society
· Past president and honorary lifetime member of the International Society for Technology in Arthroplasty (ISTA)
· Member of the review panel at DEKRA; DEKRA is a notified which ensure CE-marking of (orthopaedic) products
· Elected member of the European Knee Society
· Elected member of Academia Europea
· Board member of the Committee for Science for the Dutch Orthopaedic Association
· Member of the ERC starting grant evaluation panel (LS7); ERC Diagnostic Tools, Therapies and Public Health.
· Editorial board member of the Bone & Joint Journal (Br.)
· Consultant for Invibio Ltd (UK) to design a polymer total knee replacement
· Consultant for Exactech (USA) to design a new tibial component
· Awarded to present the Erwin Morscher Honorary Lecture at the European Federation of National Associations of Orthopaedics and Traumatology (EFORT) meeting in Vienna (2017)
· Winner of the 5th Grand Challenge Competition at the World Congress of Biomechanics (2014)
· Recipient of European Research Council Grant Advanced Grant, entitled: ‘Biomechanical diagnostic, pre-planning and outcome tools to improve musculoskeletal surgery’ (BioMechTools) (2013)
Research Line
Prof. Verdonschot has been working in the field of biomechanics for over 30 years. His expertise is on computer modeling of the musculoskeletal system of the human body. Using multi-modal imaging techniques (ultrasound, MRI, CT, X-Ray) computer models of a human body can be generated. With these models muscle activation patterns and forces can be estimated. These activation patterns can be compared to EMG-sensors on the body in order to validate the predictions. Furthermore, forces in joints which are predicted by the personalized models can be compared to forces measured with sensors which are embedded in joint implants.
The force generating capacity of muscles depend on the quality and adaptation of the muscle tissue. In aging subjects or patients suffering from cardiovasculair, metabolic, cancer, or neurodegenerative diseases, muscle tissue is considerably affected. Verdonschot is expert in adaptation processes of human tissues. Currently he is leading a project to assess muscle adaptation processes in amputation patients. Using new MRI sequences in combination with semi-automated segmentation techniques his group is quantifying the effects of re-training muscles in amputation patients.
In another project the reduction of the force generating capacity of facioscapulohumeral dystrophy (FSHD) patients was measured and simulated as compared to healthy controls. FSHD is a muscledisease showing fattening of the muscle tissue, thereby the force generating capacity. By combining ultrasound and MRI technologies the behavior of these muscles can be studied under in-vivo conditions. Verdonschot recently showed that even the healthy parts of the muscles in FSHD patients have inferior quality.
Verdonschot led a large EU project (TLEMsafe) in which he generated predictive tools to assess the functional outcome in patients with cancer in the musculoskeletal system. In these patients often muscle tissue is removed and it remains questionable what the functional recovery will be after surgery. With the models generated by the group of Verdonschot these predictions can be made. Using a virtual reality pre-planning system, the surgeon can execute the surgery on the model (before performing the actual one). The model predicts the functional effects of the surgery and the surgeon can decide together with the patient whether the functional outcome is acceptable or whether for example an amputation should be considered. The functional outcome of these patients can be evaluated with actual measurements on patients using motion and force sensors.
Bart Kaptein 1
1Leiden University Medical Center, Department of Orthopaedics
Email: B.L.Kaptein@LUMC.nl
Wear of the polyethylene insert in Total Knee Arthroplasty (TKA) is a problem as the wear particles cause osteolysis that may lead to implant loosening[1]. The introduction of new highly cross linked polyethylene (XLPE) has reduced the wear rate of TKA inserts to a great extent. Even though, there are still concerns with regards to the mechanical properties of XLPE introduced by irradiation and thermal treatment of the material. For these reasons, highly accurate in vivo TKA wear measurement methods are necessary.
With Model-based RSA, it is possible to accurately measure the position and orientation of the tibial and femoral components in TKA from a calibrated stereo radiograph[2]. Based on this 3D reconstruction of the prosthesis it is possible to measure the minimum joint space width (mJSW) on both condyles. The change in mJSW over time defines the linear wear rate[3]. Volumetric wear may be measured by introducing a 3D model of the insert and measure the overlap between the femoral component and the insert[4] (Figure 1).
In this presentation, an overview of the different methods of in vivo wear measurements will be presented. The validation results of phantom experiments will give an overview of the accuracy and precision of these measurements. In addition, the results of in vivo clinical studies will be used to investigate the differences between linear and volumetric wear.
1. Jacobs, J.J., et al., Osteolysis: basic science. Clin Orthop Relat Res, 2001(393): p. 71-7.
2. Kaptein, B.L., et al., A new model-based RSA method validated using CAD models and models from reversed engineering. Journal of Biomechanics, 2003. 36(6): p. 873-882.
3. van Ijsseldijk, E.A., et al., The robustness and accuracy of in vivo linear wear measurements for knee prostheses based on model-based RSA. Journal of Biomechanics, 2011. 44(15): p. 2724-2727.
4. van Ijsseldijk, E.A., et al., Validation of the in vivo volumetric wear measurement for total knee prostheses in model-based RSA. Journal of Biomechanics, 2013. 46(7): p. 1387-1391.
Bart Kaptein studied Mechanical Engineering at the Technical University of Delft. In 1999 he finished his Ph.D. thesis in Delft entitled: "Towards in vivo parameter estimation for a musculoskeletal model of the human shoulder". Since 2000 he is working at the Biomechanics and Imaging Group of the Department of Orthopaedic Surgery at the Leiden University Medical Center as a senior researcher on projects together with the Image Processing group of the Department of Radiology.
His main interests are in measuring in vivo prosthesis motion, migration and wear.
He is the main developer of the Model-based Roentgen Stereophotogrammetric Analysis (MBRSA) system. With Model-based RSA, micromotions of orthopaedic implants with respect to the bone are measured, which is a predictor for early failure of the prosthesis.
He is the Managing Director of RSAcore, which is part of the Department of Orthopaedic Surgery of the LUMC. RSAcore works on the development and exploitation of the Model-based RSA system and provides support for clinical RSA studies.